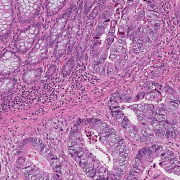
Mirxes Corporation USA, a fully-owned subsidiary of Mirxes Pte Ltd, an RNA technology startup headquartered in Singapore, has revealed that their pioneering product, GASTROClearTM, an in vitro diagnostic test utilizing PCR-based technology, designed for the early recognition of gastric (stomach) cancer, has been accorded the distinguished Breakthrough Device Designation by the US Food and Drug Administration (FDA).



This development signifies a global milestone as it’s the first instance where three significant achievements have converged: 1) an innovative blood miRNA test, 2) an in vitro diagnostic (IVD) tool aimed at the early detection of gastric cancer, and 3) a molecular in vitro diagnostic assay originating from Southeast Asia, all of which have been awarded the esteemed Breakthrough Device Designation by the US FDA. This recognition is exclusively bestowed upon select medical devices that address unmet necessities and deliver heightened efficacy in treating or diagnosing life-threatening or irreversibly debilitating illnesses like cancer.
Unveiled back in 2019, GASTROClearTM holds the distinction of being the planet’s maiden molecular blood examination devised to spot early signs of gastric cancer, empowering both medical practitioners and patients to take proactive measures well before the manifestation of symptoms. The journey of GASTROClearTM’s development and production spans seven years, nurtured by the collaboration of scientists and physicians from esteemed institutions such as the Agency for Science, Technology, and Research (A*STAR)’s Bioprocessing Technology Institute (BTI), Diagnostics Development Hub (DxD Hub), the Singapore Gastric Cancer Consortium (SGCC), the National University of Singapore (NUS), the National University Hospital (NUH), Tan Tock Seng Hospital (TTSH), and Mirxes.
The Singapore Health Science Authority (HSA) granted its approval to GASTROClearTM in 2019 after a prospective clinical validation encompassing more than 5,200 patients within Singapore. In a more recent development, Mirxes, in partnership with seven academic clinical institutions in China, undertook an extensive prospective clinical trial involving over 9,000 patients to secure the registration of GASTROClearTM with China’s National Medical Product Administration (NMPA). Post the pandemic, Mirxes is actively facilitating access to GASTROClearTM in key Asia Pacific markets while simultaneously exploring collaborations to facilitate its introduction within the United States.
As of now, GASTROClearTM is accessible in Southeast Asian markets including Singapore, Indonesia, Malaysia, and the Philippines.